Foundations of Ultrasonics for Dental Hygiene Students

Teaching theoretical and clinical ultrasonic technology to the next generation of dental hygiene professionals does not have to be complicated. In fact, with the tools that this blog series will cover, you will be well prepared to incorporate an enriched contemporary ultrasonic curriculum that will prepare your students to practice 21st century dental hygiene.
In this blog series, I take best practices and tools from my textbook, Power Instrumentation for the Dental Professional, to provide important overviews of ultrasonic foundations, ultrasonic curriculum and instrumentation technique, and chairside student coaching and teaching.
Let’s start by reviewing ultrasonic infection prevention, mechanism of action, and fluid dynamics.
Teaching Aerosol Protection is Critical to Student Safety
Power Instrumentation for the Dental Professional teaches the most current recommendations for provider aerosol protection in chapters 1 and 2. This foundational knowledge is of the utmost importance given the SARS-CoV-2 infection rates still present in most countries.
Dental ultrasonics and air polishers expel at minimum half-a-million small sized aerosol particles into the environment that will travel up to 10 feet both horizontally and vertically.
Periodontal debridement produces the highest number of aerosols compared to any other dental procedure.
Bioaerosols contain blood, viruses, and bacteria from the patient’s mouth and dental unit waterlines that can transmit disease if proper mitigating steps are not in place.
 HVE use during ultrasonic instrumentation is one of the most important tools for aerosol protection. An HVE is defined as any device that removes at minimum 100 cubic feet air per minute.
HVE use during ultrasonic instrumentation is one of the most important tools for aerosol protection. An HVE is defined as any device that removes at minimum 100 cubic feet air per minute.
Just because a device connects to an HVE line, does not make it an HVE!
Provider mask selection for an aerosol-generating procedure is extremely important to protect the wearer’s respiratory pathways and decrease the risk for disease transmission via aerosol entry through the nose and mouth.
A filtering facepiece respirator (FFR) mask (N95) combined with a face shield is recommended by the CDC and WHO. A face shield protects the wears skin and outer layer of the mask from moisture. Mask effectiveness decreases when it becomes wet due to wicking. Aerosol and splatter droplets heavily contaminate a provider’s face, neck, arms, and chest during procedures.
According to the WHO, “Surgical masks, regardless of the level, do not provide adequate respiratory protection from small size aerosol particles, are not certified as respirator masks by NIOSH, and do not satisfy OSHA requirements for respiratory protection during aerosol-generating procedures.”
Chapter 2 also presents current literature on pre-procedural rinsing, ventilation, air decontamination, and line maintenance to maintain the highest safety standards for dental aerosol-generating procedures.
Why Should I Teach Students the Mechanism of Action of Ultrasonics?
Students should recognize, understand, and appreciate the mechanism of action of any device, tool, or instrument before they use it for the first time. For example, in radiology, we teach radiation physics and ionizing radiation safety before a student exposes a radiograph on a human to keep everyone safe. In preclinic, we teach soft tissue anatomy and periodontal probe design before a student places the instrument subgingivally on a patient.
The same applies in ultrasonic curriculum. Students must understand device design, functionality, and action so they can make sound clinical decisions and safely operate the equipment.
What is a Dental Ultrasonic?
In a nutshell, all dental ultrasonics are energy transmitting devices made of a transducer and active medium.
Transducer/Converter: Transforms electric energy into mechanical energy through the formation of ultrasonic waves (red/blue waves). There are 2 transducers used in dentistry:
- Piezoelectric: active medium is PZT (lead-zirconate-titrate) discs (located in the handpiece).
- Magnetostrictive: active medium is nickel (located on the insert).
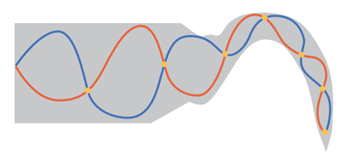
When the two ultrasonic waves collide with one another – a nodal point (orange dots) is formed.
- Nodal points = Site of no activity.
-
Location: 3.5-5mm on the shank.
-
Never adapt this area of the shank on a tooth because deposits will not be removed.
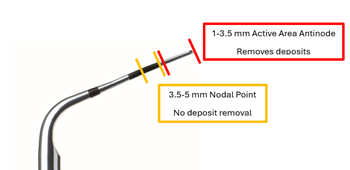
Adapt the active area antinode to a tooth surface for deposit removal

Blue arrow pointing to the nodal point
Ultrasonic Mechanism of Action
Learning the fluid dynamic mechanism of action of an ultrasonic is easier than you think and quite interesting given its profound microbiological effects in the mouth.
When my son blows bubbles through a straw into a glass of milk and creates bubbles, that’s a great example of creating the fluid dynamic called cavitation.
Cavitation is simply the formation of a bubble inside a liquid, like my son’s milk. A dental ultrasonic produces the same thing except our ultrasonic shanks release millions of acoustic (sound) cavitational bubbles when we step on the pedal. You can see the bubbles on my student’s typodont.
What’s so Special about Acoustic Cavitation Bubbles?
These bubbles possess amazing capabilities. They are full of kinetic energy and vapor gas as described in the video.
When bubbles are produced by a dental ultrasonic, they are called acoustic (sound) cavitational vapor gas bubbles because they are formed in a liquid that contains sound waves.
The bubbles interact with each other in the liquid rolling about itself (oscillating via primary Bjerknes forces), bumping into one another and repelling off one another (via secondary Bjerknes forces).
Internally, they have so much kinetic energy, they create mini tornadoes inside of them called liquid jets. The liquid jet will jump out of the bubble when fully formed and release energy for the formation of more acoustic cavitation vapor gas bubbles and pierce a bacterial cell wall leading to destruction.
The bubbles are carried in an acoustic microstreaming current inside the mouth and travel away from the ultrasonic shank. If you look at my student’s typodont image – their shank is adapted to the LR 1st premolar, but you see acoustic cavitation bubbles on the HVE mirror, tongue, and surrounding teeth.
The bubbles do not live forever. Eventually they will implode inside the mouth – and when they do – WATCH out because this is when profound microbiological changes occur that differentiate power debridement from hand-activated debridement.
What Oral Effects Occur During Ultrasonic Instrumentation?
When a bubble implodes, it releases an intense shock wave in the mouth that can:
Cause microfractures on bacterial cell walls which leads to cell death.
Detach adherent biofilm from tooth surfaces without contact. Latest research has shown biofilm removal when the shank is up to 2-3mm away from the complex.
Acoustic streaming deforms bacteria cell walls through hydro (water) dynamic shear (to cut or break) stress which leads to cell death. Liquid jet tornadoes piece bacterial cell walls which leads to cell death.
If you’re interested in learning more about ultrasonic foundations, check out Power Instrumentation for the Dental Professional. Dental hygiene instructors can download a digital review copy for free!
Stay tuned for parts 2 and 3 of this blog series!
Power Instrumentation for the Dental Professional with Navigate Advantage Access First Edition
Power Instrumentation for the Dental Professional aims to bridge the gap of knowledge between education and clinical practice by allowing the student to acquire the knowledge needed to implement power technology effectively into patient care with a contemporary approach to preventive, maintenance, and non-surgical periodontal procedures.
Instructors: Learn More